Trans men who’ve been on testosterone can be just as fertile as cis women, landmark study finds

The new study from Boston IVF shows that trans men have similar egg yields as cis women do (Envato Elements)
A groundbreaking new study on transgender fertility has proven that hormone therapy does not impact egg yields for trans men.
The study was led by researchers and reproductive endocrinologists at Boston IVF, a worldwide leader in fertility care and a pioneer in LGBT+ families.
It is the largest ever study to investigate the clinical results of transgender male patients undergoing fertility preservation, and the first ever to describe transgender IVF cycle parameters in such detail and scope.
Experts analysed eight years of patient data from 25 trans men, more than half of whom had been on testosterone therapy before undergoing standard egg stimulation treatment. All had discontinued testosterone therapy for an average of four months before starting treatment.
The exciting results proved that trans men have similar egg yields to cisgender women who’ve never taken testosterone – meaning they can be expected to have a similar success rate with IVF as their cis female counterparts, even if they’ve been on testosterone for years.
“Our study found that even long periods of gender-affirming androgen therapy did not appear to have a negative effect on ovarian stimulation outcomes,” said Boston IVF Reproductive Endocrinologist Nina Resetkova, MD, MBA.
“Based on these results, our goal is to continue encouraging patients to evaluate their options before starting testosterone therapy – but also reassure individuals that if you are on hormones – you still have good options to preserve your fertility or start a family.”
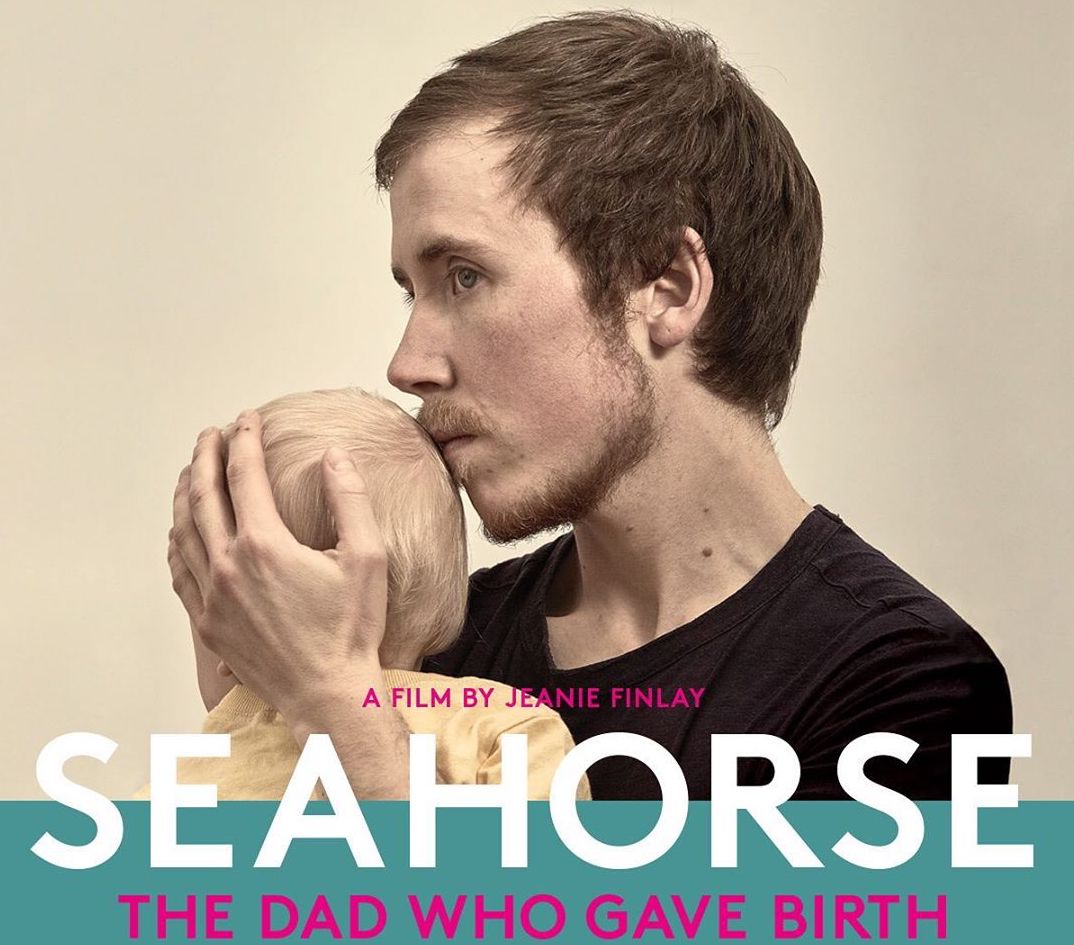
Freddy McConnell’s pregnancy journey was documented in the groundbreaking film Seahorse. (Instagram/@SeahorseFilm)
Trans men’s ability to conceive and carry a child has been well documented over the years, but never in the context of a scientific study such as this.
The results fly in the face of the conventional wisdom that transgender men need to freeze eggs before starting testosterone in order to have children one day.
But for those trans men who do want to freeze their eggs, the study reassures them that they should have the same clinical outcomes as cis women.
“I think there is a giant myth that testosterone turns your ovaries into papier-mâché,” said Dr Johanna Olson-Kennedy, medical director of the Centre for Transyouth Health and Development, speaking to NBC.
“I think these studies that are coming out are saying that’s not true, actually. Actually, they are more like hibernating.”
Questions remain about whether the results would apply to trans men who used puberty blockers in their youth, although experts maintain that this doesn’t cause infertility either.
Olson-Kennedy said that trans men who took puberty blockers should, in theory, be able to go through an endogenous puberty if they stop taking testosterone to become pregnant.
“We don’t know because no one has ever done it,” she said. “I mean, it stands to reason that somebody would, because your hypothalamus doesn’t change – you’re still secreting the same hormones that you would otherwise, you’re just significantly delayed.”
While egg freezing is still an option for dysphoric teens who want to go on puberty blockers, it will be reassuring to know that other routes to fatherhood may be available to them in future if they choose it.
“For young patients looking to transition, there needs to be more support and knowledge offered when it comes to their reproductive options for the future,” said Boston IVF reproductive endocrinologist Samuel Pang, MD.
“We hope that studies like ours will assist providers in counselling transgender individuals, to inform them that they have a great chance to have children through assisted reproductive technologies.”