HIV doctor whose life-saving antibodies were refused because he is gay says UK’s ‘humiliating’ blood ban is fundamentally wrong

Dr Joseph Heskin, a sexual health and HIV specialist, was told his sexuality made him ineligible for blood donation (BBC 5 Live)
A gay doctor who survived coronavirus has described his humiliation at being told his sexuality made him ineligible to donate his potentially lifesaving blood plasma.
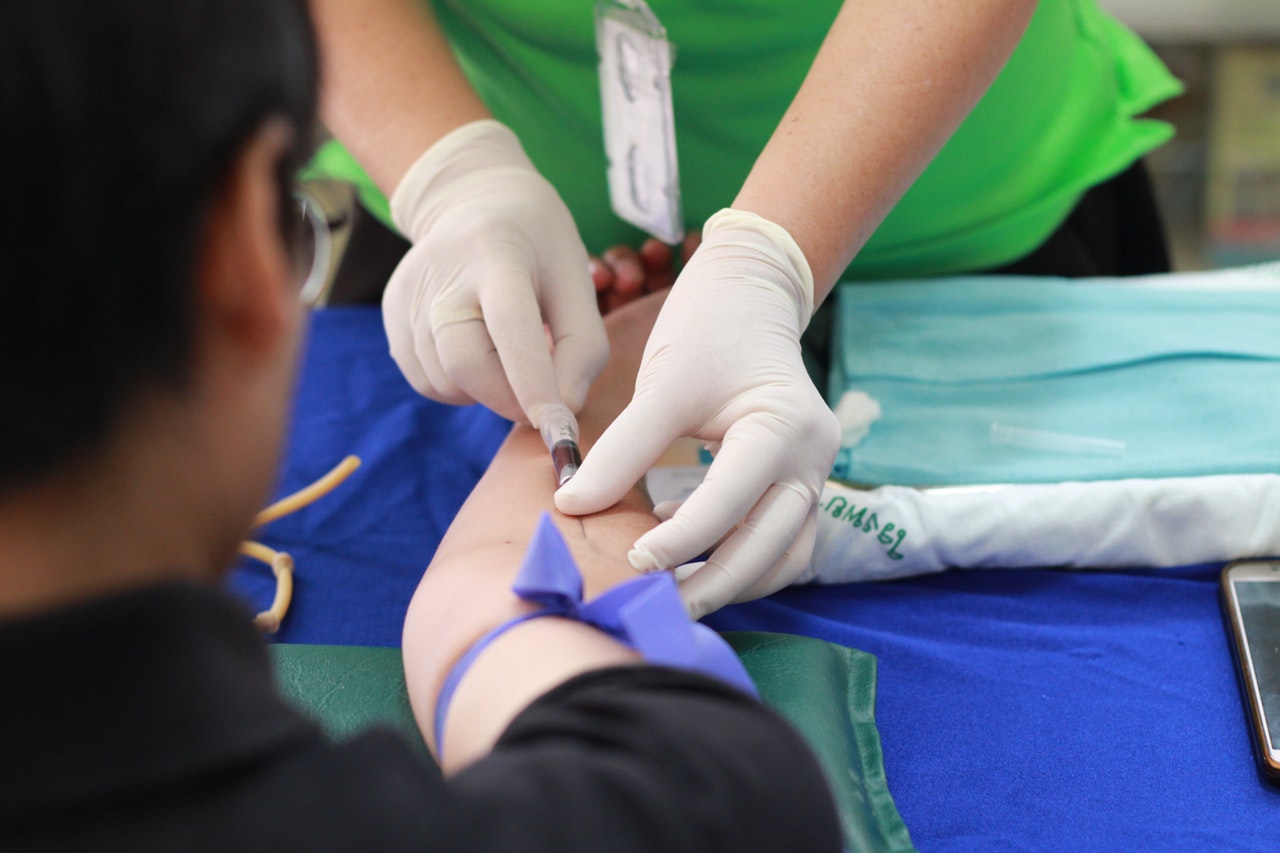
Joseph Heskin is a sexual health and HIV doctor who contracted coronavirus while working on a COVID-19 ward. When he recovered he volunteered to donate his blood plasma, which contains coronavirus antibodies, to help treat other patients with the virus.
He was devastated to learn that this wouldn’t be possible because of the UK’s discriminatory blood donation restrictions against gay and bisexual men.
“It was honestly quite humiliating,” he told BBC 5 Live. “It made me feel like I did when I was younger and I wasn’t comfortable with my sexuality, and I was ashamed and embarrassed.
“It was quite strange because I knew that the answer I was given was coming, because I’ve spoken to other people who have been through the same process. So I actually expected that answer and yet still it took me by surprise how upsetting it was.”
The original lifetime ban and subsequent restrictions for gay and bisexual blood donations are based on outdated guidelines from the start of the HIV epidemic.
Working as he does in sexual health, Heskin knows better than most that these restrictions are arbitrary at best, and discriminatory at worst.
“When you realise that within your own professional environment, within the organisation that employs you, there are criteria that deem you [and] your blood an unacceptable risk to the public — even though I know as myself but also as a clinician, as a HIV physician, that that just isn’t true — to be made to feel dirty or unclean, it brings all the [shame] rushing back again,” he said.
While Heskin accepts that the Department of Health’s current policy aims to maintain a safe donation pool, and fully supports this aim, he explains that the justification for it is fundamentally wrong.
“It’s based on what they perceive as high risk groups for blood-borne viruses such as HIV and hepatitis, and that’s based on people’s sexual practises,” he said.
“[But] if you have a man who has been married for 20, 30 years, someone who’s in a monogamous relationship, hasn’t had a partner in however many months or years, they’re offering no greater risk of HIV to a blood donation pool than a heterosexual person who’s also married or also in a monogamous relationship.”
He’s now speaking out about his experience to bring attention to the flaws in the UK’s current blood donation policy, and urge for its reform.
“What we’re saying is that the blood transfusion criteria are not accounting for heterosexual individuals who may have multiple sexual partners, may not be using any form of barrier contraception or additional protection – and yet there’s no barrier to them donating,” he said.
“But there’s currently barriers to gay and bisexual men donating who may be of no risk whatsoever.
“We’re asking that instead of doing a blanket ban they do an individualised risk assessment, which could amount to a handful of questions to each person when they come to donate blood.”
The result of this, he believes, would be that some heterosexual people may find themselves no longer eligible for blood donation, but a greater number of gay and bisexual men may find that they are.
The NHS is currently working with FAIR (For the Assessment of Individualised Risk), a steering group that is exploring whether individualised risk assessments of potential donors could be adopted in future. It is due to report its findings by the end of the year.
“We need a donor selection system that is safe and can also cope with large numbers of people,” said Dr Su Brailsford, the group’s chair. “We need to understand which questions are most relevant to assessing risk and whether there are some questions which might put people off donating.
“This work takes time and we need to make sure everything we do is based on good evidence with patient safety as the number one priority.”
An NHS Blood and Transplant spokesperson told PinkNews that the deferral period for gay and bisexual men is part of a policy set by the Department of Health.
“We are using the current donor selection guidelines. The Government set the three month deferral. This is based on expert advice from a Department of Health and Social Care expert committee called SaBTO,” they said.
“We appreciate that any deferral is disappointing if you want to save lives by giving blood, platelets or plasma.
“We recognise that people want to be considered as individuals as much as possible. Separately to the convalescent plasma trial, we are already working collaboratively with LGBT+ groups on blood donation, through the FAIR steering group.”
They added: “We want to give as many people as possible the opportunity to donate whilst continuing to ensure the safety of patients remains our number one priority.”